Abstract
Introduction: Despite high prevalence of Sickle Cell Anemia (SCA) in sub-Saharan Africa, systematic evaluation of structural and functional impact of pediatric sickle cerebrovasculopathy has been limited. In a cross-sectional study of children with HbSS, ages 1-12 years, receiving care at the Mulago Hospital SCD clinic in Kampala, we hypothesized there would be high prevalence of multi-modal brain injury and stroke risk, as defined by 4 different adverse outcomes. Here we present our completed study results.
Methods: Patients were randomly selected from the electronic clinic roster. None was taking hydroxyurea. Exclusion criteria: acute illness, Hb <6.0gm/dl, transfusion within the prior 3 months or participation in an unrelated clinical study. Adverse outcome was defined as abnormalities in ≥1 of 4 modalities examined. Stroke examination: were performed by pediatric NIH Stroke Scale (NIHSS). Psychometric testing: Age-appropriate Mullen Scales of Early Learning or Kaufman Assessment Battery, 2nd edition for Children-II, for ages 1-4 or 5-12, respectively, performed by skilled testers using validated versions in English or a predominant local language. Abnormal results defined as >2 Z scores below age-specific established community norms. Transcranial doppler ultrasounds (TCDs): Non-imaging TCDs (SonaraTek) were performed by two study trained staff (excellent inter-operator reliability >0.85); read by a U.S.-certified co-investigator. Brain magnetic resonance imaging (MRI), including arterial imaging (MRA): Subset of 81 (30.1%) of subjects (n=81), enriched for 1 or more testing abnormality, underwent non-contrast MRI/MRA imaging by a single 1.5T scanner. Two radiologists performed clinical reads. Statistical methods: ANOVA, multivariate, chi square, logistic regression.
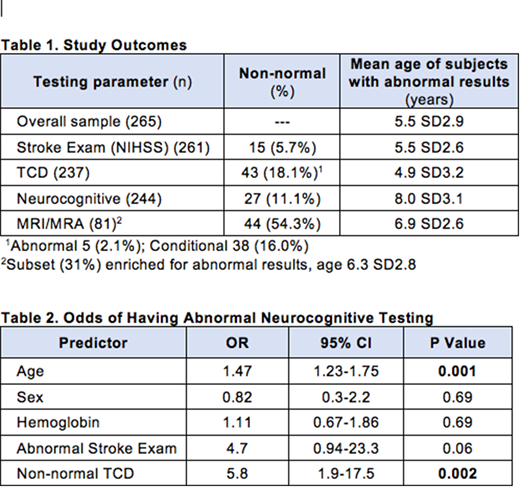
Results: Of 287 patients screened, all 265 eligible subjects were enrolled. Mean age was 5.5 SD 2.9 years, 52.3% male (Table 1). Mean Hb was 7.3 SD1.0 gm/dl. Each outcome was normally distributed.Stroke exam: Results: see below. Neurocognitive results: Overall results: see below. Poor testing: 2 of 100 ages 1-4 (2.0%) and 25 of 144 ages 5-12 (17.4%). TCDs: 13 of 251 (5.2%) were unread due to inadequate bone windows (12), poorly cooperative subject (1). Overall results: see below. MRI/MRAs: Overall results: see below. Abnormalities ranged from multiple small infarcts to multiple, bilateral infarcts and multi-vessel arterial stenoses. Among those with abnormal MRI/MRA, 13 (29.5%) also had a non-normal TCD. Summary data: In all, 58 (21.9%) subjects had ³1 abnormal outcomes. Among the 81 subjects with MR imaging, 28 (34.6%) had ³2 abnormal outcomes: 18 had 2; 9 had 3; 1 had all 4. Analyses: Abnormal neurocognitive results were highly dependent (6.8-fold) on age (<0.001) (Table 2). Abnormal MR imaging was associated had a 3-fold with abnormal neurocognitive results (0.034), but not significant when adjusted for age.
Conclusions: These data demonstrate early, frequent neurovascular pathology for each outcome tested. Abnormal neurocognitive test results significantly increased with age or non-normal TCD. Our findings provide a baseline for longitudinal assessment and incentive for intervention. Enhanced research capacity was gained for junior faculty, trainees and staff, in areas of the conduct of brain research and focus on pediatric SCD, TCD performance and neuro-epidemiology.
Funding: 1R21HD089791 (PIs: Idro, Green)
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal